Part 7 of 49 - Video Presentations of the "1st Conference on Integrating Early Detection of Heart and Lung Disease through Low-Dose CT": Day 1 Session 1: Heart Failure
- Jan 7, 2025
- 9 min read
Thursday, September 19, 2024 | New York Academy of Medicine (NYAM)
1216 5th Ave, New York, NY 10029
Dr. Sean Pinney emphasized the critical role of early detection in preventing heart failure-related deaths. He discussed the high prevalence of heart failure, a condition characterized by symptoms due to cardiac abnormalities and elevated natriuretic peptide levels, and the disparities in its impact across different populations. In addition, Dr. Pinney highlighted various screening methods, including natriuretic peptide testing, echocardiograms, and AI-enhanced tools, to identify and manage at-risk individuals more effectively.
Watch Dr. Sean Pinney's Presentation Below:
See Dr. Sean Pinney's Slides Below:
-
Expand to Read the Text Transcript
Transcript of Dr. Sean Pinney's Presentation:
[Sean Pinney] [0.24s] Thank you very much.
[Sean Pinney] [0.96s] Thanks for the opportunity to speak today about how we can avert premature death from heart failure, through early detection.
[Sean Pinney] [7.44s] These are my disclosures.
[Sean Pinney] [8.48s] So if we're gonna go look for something, we have to define exactly what is it we're screening for.
[Sean Pinney] [12.80s] So let's start with the universal definition of heart failure.
[Sean Pinney] [16.07s] So heart failure is a clinical syndrome.
[Sean Pinney] [18.16s] It's not a specific disease.
[Sean Pinney] [19.75s] It's a syndrome and it's defined by having symptoms or signs caused by a structural and or functional cardiac abnormality.
[Sean Pinney] [28.80s] And this has to be accompanied by one of 2 things.
[Sean Pinney] [32.16s] There has to be either elevated natriuretic peptide levels or there has to be objective evidence of congestion, either pulmonary congestion or systemic congestion.
[Sean Pinney] [41.44s] And then from that definition, we go a little bit further and we define 4 distinct stages of heart failure.
[Sean Pinney] [47.05s] We're not very creative.
[Sean Pinney] [48.01s] It's a, b, c, d.
[Sean Pinney] [49.45s] A are those patients who are at risk for developing heart failure, hypertension, diabetes, obesity.
[Sean Pinney] [55.45s] Patients who have stage b heart failure define as having typically think about with heart failure, symptomatic patients who have breathlessness.
[Sean Pinney] [70.78s] What we typically think about with heart failure, symptomatic patients who have breathlessness and congestion and then advanced heart failure are those patients with end stage heart failure.
[Sean Pinney] [79.58s] Now when I was growing up, the risk of experiencing heart failure was 1 in 5, about 20% lifetime risk of developing heart failure.
[Sean Pinney] [88.52s] And as we heard this morning from doctor Harrington, things are getting worse.
[Sean Pinney] [91.72s] The risk now is 24%.
[Sean Pinney] [93.80s] One out of every 4 individuals in the United States will experience heart time over heart failure over their lifetime.
[Sean Pinney] [100.92s] But let's look at it by stages.
[Sean Pinney] [102.76s] And if we look at those patients who have subclinical or preclinical disease, either stage a or stage b, 50% of Americans over the age of 20 will experience heart failure in their lifetimes.
[Sean Pinney] [116.82s] Think about that for a minute.
[Sean Pinney] [118.26s] 50% of Americans will have heart failure over their lifetime.
[Sean Pinney] [122.42s] And that's like taking this half of the room and say, okay.
[Sean Pinney] [124.98s] You guys are gonna have heart failure, and you guys will not.
[Sean Pinney] [128.18s] That's how prevalent heart failure is.
[Sean Pinney] [130.90s] When we look at it a little bit more, about 30% have stage a who have risk factors for heart failure, and about 25 to 30% are stage b who have structural disease, but are asymptomatic.
[Sean Pinney] [144.29s] Now this burden is not equally shared.
[Sean Pinney] [146.37s] In fact, there are disparities in individuals who have heart failure.
[Sean Pinney] [149.89s] The fact that incidence of heart failure is about twice as high for black Americans as it is for white Americans, and the risk is somewhere in between for Hispanic Americans.
[Sean Pinney] [162.86s] Failure disproportionately felt, but so is mortality from heart failure.
[Sean Pinney] [166.14s] And this is true that over 2012 to the current time, deaths from heart failure are increasing, but that burden is disproportionate for black men as compared to white men and white women.
[Sean Pinney] [179.24s] And we also can see disparities when we look across the country when we go county by county, and you'll see that the risk of dying from heart failure is greatest in the southeast, in the south, and in the Midwest.
[Sean Pinney] [189.67s] And if you were to zone in on urban centers like New York or San Francisco or Chicago, you'll see that the rates of dying from heart failure are actually the lowest in the country.
[Sean Pinney] [199.50s] So what are we talking about?
[Sean Pinney] [200.54s] We're talking about access to health care.
[Sean Pinney] [202.46s] And this is important when we think about screening modalities.
[Sean Pinney] [205.82s] How are we going to get screening tests to the patients who are at greatest risk of experiencing heart failure.
[Sean Pinney] [212.94s] This is particularly true for those individuals who live outside urban areas who live in in, in the country.
[Sean Pinney] [221.09s] So what is the current state of affairs?
[Sean Pinney] [222.94s] How do we diagnose heart failure?
[Sean Pinney] [224.29s] Believe it or not, this is one way to do it.
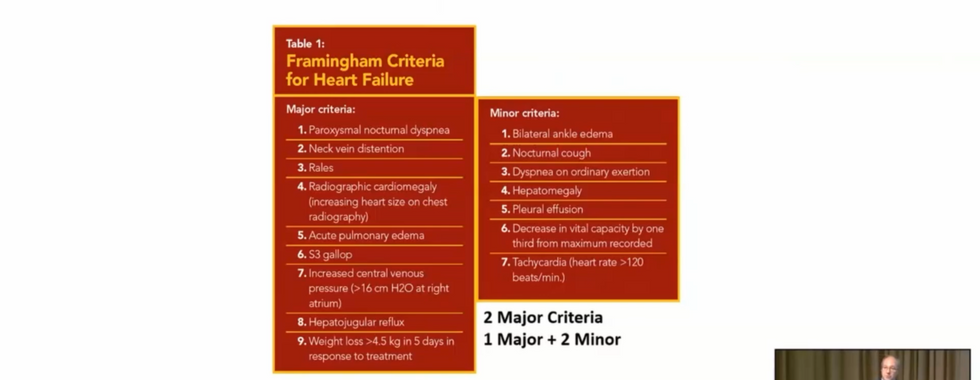
[Sean Pinney] [226.29s] This is endorsed by the guidelines.
[Sean Pinney] [227.53s] You use the Framingham criteria.
[Sean Pinney] [229.21s] You need 2 major criteria or 1 major criteria and 2 minor criteria.
[Sean Pinney] [232.97s] Nobody does this.
[Sean Pinney] [234.09s] But if you look at the criteria, what those are, those are actually signs and symptoms of congestion.
[Sean Pinney] [238.57s] But we can take this model, and we can assign points for the presence or absence of each one of these particular factors.
[Sean Pinney] [245.11s] And this multivariable model actually does pretty well in predicting the risk of incident heart failure over the next 4 years.
[Sean Pinney] [252.16s] And we can improve this model, and this was done through ERIC, the atherosclerotic risk and communities database by adding natriuretic peptides.
[Sean Pinney] [260.68s] And this significantly improves the predictive ability of the model.
[Sean Pinney] [265.32s] However, this is not really clinically applicable.
[Sean Pinney] [268.88s] But embedded in this is a little nugget, and the nugget is the fact that congestion, particularly elevated natriuretic peptide levels, can be particularly effective in screening populations who are subclinical.
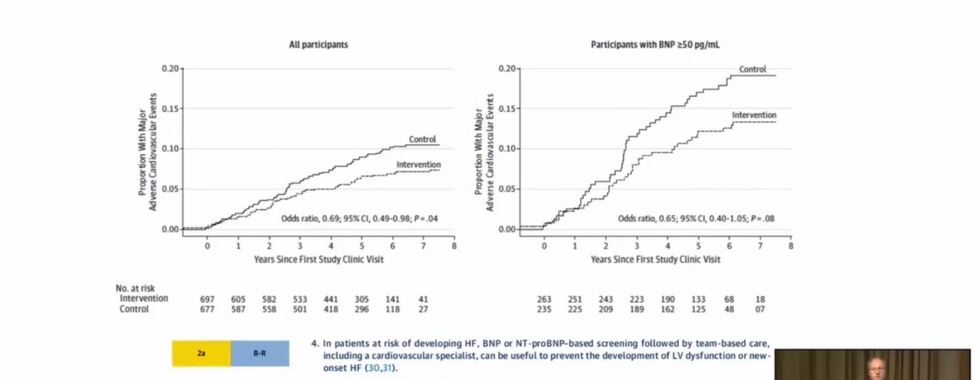
[Sean Pinney] [281.31s] And this was the basis for the most aptly named trial, which was called the stop heart failure trial.
[Sean Pinney] [286.19s] This was conducted throughout multiple primary care practices in Ireland with a simple premise.
[Sean Pinney] [291.55s] They took individuals who did not have any heart failure, symptomatic heart failure, but were at risk.
[Sean Pinney] [296.65s] So those stage a, stage b individuals, and they drew natriuretic peptide levels.
[Sean Pinney] [301.05s] And if you had an elevated b and p level greater than 50, not that high, you were then randomized to have an echocardiogram and a consultation with a cardiologist.
[Sean Pinney] [309.77s] It cut the incident the rate of incident heart failure in half, and it also improved survival in those individuals who were treated with a RAS antagonist and followed with a cardiologist.
[Sean Pinney] [321.05s] And for that reason, it's now in the guidelines.
[Sean Pinney] [322.97s] In the current, ACC guidelines for treating heart failure, it's a two way recommendation that patients who are at risk for having heart failure should be screened with natriuretic peptide levels.
[Sean Pinney] [334.12s] But let's take that concept of congestion a little bit further.
[Sean Pinney] [337.40s] Not everyone has access to natriuretic peptide level testing, but a lot of places have ultrasound.
[Sean Pinney] [343.10s] This was a study a substudy of the OMID trial, which looked at those at risk patients against subclinical, no history of, any heart failure symptoms and assigned them to have a screening echocardiogram.
[Sean Pinney] [355.10s] 3 fourths of them happen to have elevated natriuretic peptide levels.
[Sean Pinney] [358.56s] They then looked at jugular venous distension, IVC collapsibility, and lung ultrasound to look for curly b lines.
[Sean Pinney] [365.93s] And what they found was about 30% of those individuals completely asymptomatic had evidence of congestion.
[Sean Pinney] [371.81s] And when they dug a little bit deeper, what they found was that it correlated with having higher natriuretic peptide levels and also larger left atrial volume, something that we heard today about screening and using CT scan for that, which then raises the question, is this a better prognostic marker for development of incident heart failure?
[Sean Pinney] [389.38s] And is this something that can be substituted in those areas where natriuretic peptide testing cannot be performed?
[Sean Pinney] [396.47s] Well, keeping with that congestion thing, we know that before you have overt congestion in the lungs or in the legs, we know that hemodynamic profile rises.
[Sean Pinney] [406.39s] And we can detect this now with an implantable cardiac sensor called the CardioMEMS device.
[Sean Pinney] [412.50s] And this is a very sensitive device to look for changes in pulmonary arterial pressure, that correlates with left atrial pressure, and we can act on patients who have a history of heart failure.
[Sean Pinney] [423.04s] The problem with this is, clearly, it's not for everyone.
[Sean Pinney] [425.52s] It's not scalable.
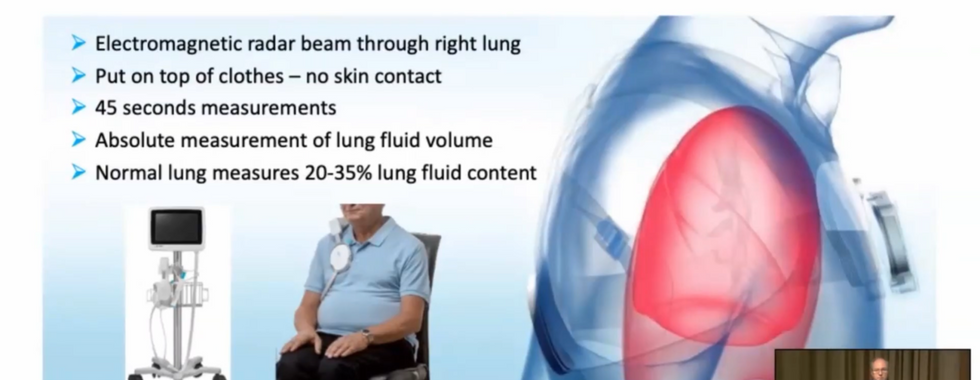
[Sean Pinney] [426.88s] But there are other things that are noninvasive ways of detecting congestion.
[Sean Pinney] [430.32s] This is one example.
[Sean Pinney] [431.36s] This is the remote dielectric sensing or REDS Vest that is very accurate in detecting and measuring, lung fluid content.
[Sean Pinney] [440.25s] And this is something that could be applied in a internal medicine practice or a cardiology practice.
[Sean Pinney] [446.50s] It can go over the close.
[Sean Pinney] [447.45s] It takes 45 seconds to do a reading.
[Sean Pinney] [449.54s] And if you detect lung congestion, that'd be a great screening tool for the development of or screening for incident heart failure.
[Sean Pinney] [456.76s] But what about this?
[Sean Pinney] [457.64s] This is even better, which is there's a saying in medicine, listen to your patient.
[Sean Pinney] [462.20s] They're telling you what's wrong with them.
[Sean Pinney] [463.72s] Well, can we use an app?
[Sean Pinney] [466.31s] Everything's got an app nowadays.
[Sean Pinney] [467.83s] Can we make an app that can use remote speech monitoring to detect early signs of congestion?
[Sean Pinney] [474.39s] And this, in fact, is the Corteo Hero device.
[Sean Pinney] [477.36s] This is something that is now currently in clinical trials.
[Sean Pinney] [480.54s] The community study looked at this in patients who had symptomatic heart failure.
[Sean Pinney] [484.86s] Patients were asked to say a couple sentences every morning, and you can check their speech patterns.
[Sean Pinney] [490.70s] You can detect the early form of congestion and intervene earlier.
[Sean Pinney] [495.63s] And then lastly, let's turn to artificial intelligence.
[Sean Pinney] [498.19s] This is really nice work from Yale.
[Sean Pinney] [500.44s] They looked at looking at electrocardiograms.
[Sean Pinney] [503.48s] They built their model looking at 12 lead EKGs, but they extended it by looking at a single EKG lead.
[Sean Pinney] [509.20s] I mean, think about the power of that.
[Sean Pinney] [510.56s] You can do it off of a EKG lead for patients who come to the emergency room, who get an office EKG, or wear it on their eye watch.
[Sean Pinney] [518.16s] They built this model, and what they found was that when they applied this to an at risk subclinical population, patients who fit the model had a 3 to 7 fold higher risk of developing incident heart failure.
[Sean Pinney] [531.36s] And then lastly, we also know that we can use AI enhanced, clinical decision support systems to augment the ability to identify heart failure.
[Sean Pinney] [541.56s] This is just one example where they use this model to help internal medicine doctors.
[Sean Pinney] [547.48s] When they compared patients who had heart failure, went to a heart failure doctor, the heart failure doctor got it right a 100% of the time.
[Sean Pinney] [553.19s] Internists got it right about 70% of the time.
[Sean Pinney] [556.00s] But when they use this AI enhanced model, they equaled that gap.
[Sean Pinney] [559.91s] They eliminated that gap.
[Sean Pinney] [561.67s] And with the use of AI, the internists were able to detect heart failure a 100% of the time.
[Sean Pinney] [567.68s] So in conclusion, there is a very, very high prevalence of adults who are at risk for developing symptomatic heart failure.
[Sean Pinney] [574.64s] Screening modalities rely on this presence of congestion.
[Sean Pinney] [577.68s] I think we can do better than that.
[Sean Pinney] [578.11s] There's clearly a need for novel approaches which are scalable.
[Sean Pinney] [578.41s] And, There's clearly a need for novel approaches which are scalable.
[Sean Pinney] [583.15s] And lastly, AI will be an essential tool to enable, screening large populations of heart failure patients.
[Sean Pinney] [589.39s] So thanks very much.
The presentations were hosted by I-ELCAP – The International Early Lung Cancer Action Program.






































Comments