Part 10 of 49 - Video Presentations of the "1st Conference on Integrating Early Detection of Heart and Lung Disease through Low-Dose CT": Day 1 Session 1: Panel Discussions
- Jan 9, 2025
- 40 min read
Thursday, September 19, 2024 | New York Academy of Medicine (NYAM)
1216 5th Ave, New York, NY 10029
Dr. Michael McConnel introduced the panelists, highlighting their expertise in coronary calcium and AI technology. The discussion focused on integrating lung cancer screening with cardiovascular prevention using low-dose CT scans. Dr. Samin Sharma emphasized the importance of clinical presentation in interpreting calcium scores, while Dr. Joseph Shemesh highlighted the genetic factors in coronary atherosclerosis. Dr. Zahi Fayad and Dr. Nathan Wong discussed the potential of AI and imaging to enhance early detection and patient adherence.
The panelists agreed on the need for further research and collaboration to optimize screening protocols and improve patient outcomes. They also stressed the importance of clear communication with patients about their CT scan results and the need for actionable recommendations. The session concluded with a call for more interdisciplinary collaboration and the development of comprehensive screening and treatment strategies.
Watch The Panel Discussion Below:
See Slides and Images from "Session 1: Averting Premature Death from Heart Disease by Early Detection" Panel Discussions Below:
_
[Michael McConnel] [0.32s] Yes.
[Michael McConnel] [0.72s] So I wanted to do some, brief introductions to other panelists, who are here.
[Michael McConnel] [9.84s] Professor Joseph Shamash is director of the Shabbat Medical Screening Center, in Israel, has 30 year experience with coronary calcium.
[Michael McConnel] [21.79s] He actually has a few slides, but with tie with the time limit we've talked about, we have another session tomorrow morning where we're gonna talk more around coronary calcium and CT scanning.
[Michael McConnel] [33.97s] So he'll generously contribute some of his, further slides on that.
[Michael McConnel] [42.23s] We have, let's see.
[Michael McConnel] [45.12s] I'll make sure I've got all my we have doctor Nathan Wong, who I've had the privilege to work with recently on with more around analyzing, a number of the Mesa data and applying AI technology.
[Michael McConnel] [59.02s] He's a professor of medicine, at, UC Irvine and directs their heart disease prevention program.
[Michael McConnel] [68.62s] And then last but not least, good friend, long time colleague, doctor Zahi Fayad, who's here at Mount Sinai, who's professor of both radiology and medicine, cardiology, also directs the Biomedical Engineering and Imaging Institute.
[Michael McConnel] [89.18s] He's has the classic image of, I think, the the first MRI scan of a vulnerable plaque in your LAD and has, been a pioneer in molecular imaging and very early in imaging inflammation in atherosclerosis, very much around highlighting that it's a biologically active disease.
[Michael McConnel] [113.06s] The New York Times still just had the thing that, you know, you need to lower cholesterol because there's this sort of stuff that builds up in your heart arteries.
[Michael McConnel] [120.74s] No no acknowledgment that it's this active biologically active disease that can, as as the first case, the 50 year old example, can strike people out of the blue, if we're not looking for it and not treating and preventing it.
[Michael McConnel] [139.28s] So once you start off, let's maybe think about what, we'll do a few questions here and then open up to the audience.
[David Maron] [151.53s] Yeah.
[David Maron] [151.85s] And I I know that, we're supposed to break at 11:30.
[David Maron] [156.09s] We're way over.
[David Maron] [158.29s] Do you think we can encroach a little on the yes.
[David Maron] [161.81s] Thank you.
[David Maron] [163.66s] So many questions have come up, I think, in all of our minds listening to these excellent presentations in this session.
[David Maron] [176.28s] Related to the question I asked from the mic before is, is there enough evidence to act on the early detection of disease.
[David Maron] [190.16s] And, I'd I'd I'd like to start, say, with with doctor Sharma, who's sitting closest.
[David Maron] [201.36s] Do you think that, CT detection of aortic valve calcification should trigger a a workup for aortic stenosis?
[David Maron] [214.80s] And and is it a certain, threshold of coronary calcium?
[David Maron] [221.75s] Do you see patients who have been detected on the basis of CT?
[Samin Sharma] [225.84s] Yeah.
[Samin Sharma] [226.16s] So question is from the valve point of view, we see see very pay the kind of young patient or for a screening point, which is more and more patients are coming to the cath lab.
[Samin Sharma] [238.13s] They're bypassing the stress test, or echo.
[Samin Sharma] [240.85s] They're getting CTA, high calcium score, or some disease, and they come to the cath lab.
[Samin Sharma] [246.03s] So that is the for coronary artery disease.
[Samin Sharma] [248.19s] But for the valve intervention, for valve point of view, they will mention if there is a calcium present.
[Samin Sharma] [254.91s] Usually, in that, actually, you expect the valve would not narrow, maybe thicken, but calcium but, yeah, there is a criteria for high calcium versus low calcium on the valve.
[Samin Sharma] [264.56s] 1200 for female and 2,000 for male will be high calcium, but that basically means it is severe.
[Samin Sharma] [270.63s] But if there is some calcium, let's say, besides the coronary calcium, and I have not seen any patient that who had only the valve calcium and there were nothing in the coronary.
[Samin Sharma] [280.24s] So once you have the valve calcium, you always will have some calcium in the coronary arteries.
[Samin Sharma] [284.64s] But, yeah, if some calcium in the aortic valve, which will trigger the next test, then test will be echocardiogram.
[Samin Sharma] [291.44s] So you do not diagnose truly the aortic stenosis by the, CT.
[Samin Sharma] [295.68s] If the echo will tell us in terms of the gradient, the the pressure gradient, the, velocity, and so and so forth, then, of course, ejection fraction will make it.
[Samin Sharma] [304.74s] So question comes back, how can we do early detection if the CT gives us some calcium on the valve?
[Samin Sharma] [311.13s] I would say yes.
[Samin Sharma] [312.34s] Let's go to the echo path, and after that, I'm, of course, beside the clinical examination, and then go further, and follow the patient based on degree of stenosis or regurgitate.
[David Maron] [325.39s] Maury, you can probably probably many of you can answer this question.
[David Maron] [329.10s] I think for men, a calcium score in the aortic valve of 3,000.
[David Maron] [334.78s] 2,000.
[David Maron] [335.34s] Is it 2?
[David Maron] [335.98s] 2,000.
[David Maron] [336.69s] 2,000.
[David Maron] [337.18s] And for women, 1200?
[David Maron] [338.86s] 1200.
[Speaker 4] [339.62s] Yeah.
[David Maron] [340.18s] Okay.
[David Maron] [340.82s] So that should suggest the presence of severe aortic stenosis and trigger a a referral to the Echolab.
[Speaker 4] [349.54s] But you're suggesting even more than that before.
[Speaker 4] [353.10s] This structure is very severe.
[Speaker 4] [354.63s] Yeah.
[Speaker 4] [355.19s] So so the question is, can we lower the threshold, and do you see benefit in those people that have lower?
[Morteza Naghavi] [364.79s] Go for a next step for a workup.
[Morteza Naghavi] [366.81s] Do you see that?
[Morteza Naghavi] [367.77s] We don't have a trial, like David said, but do you see as an expert benefit in triggering a care pathway?
[Samin Sharma] [376.09s] Yeah.
[Samin Sharma] [376.33s] So the question comes, you detected the mild, let's say, aortic stenosis by echocardiogram or by CT.
[Samin Sharma] [383.31s] So question is, what can you do?
[Samin Sharma] [385.07s] That's where the buck stops.
[Samin Sharma] [387.07s] We do not have any treatment or good treatment upstream to halt this disease progression.
[Samin Sharma] [394.27s] There have been trial trials of the statins, and they have been with the mixed results, but overall message is it does not work.
[Samin Sharma] [400.99s] Some one study showed yes, but overall and there is no other treatment.
[Samin Sharma] [404.75s] Now any of the anti inflammation, anti inflammatory will have this benefit.
[Samin Sharma] [410.13s] It still need to be seen.
[Samin Sharma] [411.25s] But what it will trigger is that you are not missing that moderate to severe AS, which patient comes one day, syncopized and in shock.
[Samin Sharma] [420.83s] So that will just trigger, that by by testing, you went back to the early stage and follow-up with the 6 month or yearly echo to follow the patients till the natural, history of the disease.
[Morteza Naghavi] [434.21s] So you think the value might be in monitoring?
[Morteza Naghavi] [437.17s] Yes.
[Morteza Naghavi] [437.65s] The disease.
[Morteza Naghavi] [438.21s] Monitoring.
[Morteza Naghavi] [438.76s] Not any inappropriate.
[Morteza Naghavi] [440.13s] Okay.
[Roxana Mehran] [440.61s] I think I think just in line with what doctor Sharma said, I think we are evolving, at the moment.
[Roxana Mehran] [447.34s] At this TCT, as you heard, early TAVR will be presented.
[Roxana Mehran] [451.02s] These are asymptomatic, mild to asymptomatic patients with aortic stenosis.
[Roxana Mehran] [456.22s] So this could maybe change that, that threshold of calcification to even lower because if there's benefit early on as doctor Sharma described, you know, maybe they're sitting in this in this curve of not just diving yet, but in this curve, they're damaging the heart muscle, everything else, and that an earlier intervention with the valve then I think will change the needle.
[Roxana Mehran] [482.85s] But I think more interesting would be to better understand, are there therapies?
[Roxana Mehran] [487.52s] I mean, we know there's some relationship between LP and aortic stenosis.
[Roxana Mehran] [492.32s] There's trials going on.
[Roxana Mehran] [494.00s] They're investigator initiated just to see where it is, with, with palacarsen.
[Roxana Mehran] [499.37s] I know there is going on, and now there are other you know, Merck and others are also and Amgen are looking at LP, therapies even in this earlier falcipic aortic stenosis.
[Roxana Mehran] [512.38s] No one really understands, but I do think that the this needle is is moving.
[Michael McConnel] [519.07s] Thanks so much.
[Michael McConnel] [521.38s] Doctor Shamesh, you, you've had a long experience with coronary calcium.
[Michael McConnel] [526.50s] It's one of the areas that still is this question as David raised early on in terms of data and outcomes in randomized trials.
[Michael McConnel] [537.20s] So how do how do we use the evidence that we have now to guide us, and what additional studies, do we do we potentially need?
[Joseph Shemesh] [547.63s] Yes.
[Joseph Shemesh] [548.20s] I think we are we are there.
[Joseph Shemesh] [551.48s] We I I think I think we are there.
[Joseph Shemesh] [554.43s] It is in the guidelines.
[Joseph Shemesh] [556.36s] I think for this form, the most important thing is that calcium score can be, evaluated by each non cardiac chest CT.
[Joseph Shemesh] [568.17s] And this is a lot of of, information that can get there, and, this is very important.
[Joseph Shemesh] [576.82s] I have one a very important comment on coronary atherosclerosis.
[Joseph Shemesh] [583.53s] Coronary atherosclerosis is not risk factor disease.
[Joseph Shemesh] [589.09s] It is a genetic disease.
[Joseph Shemesh] [591.65s] You have 2 brothers.
[Joseph Shemesh] [593.17s] I had a lot of them.
[Joseph Shemesh] [595.09s] 1 with a wonderful healthy lifestyle, and the other, just on the other side, smoking and everything, and he has zero score, and the other has a lot of calcium.
[Joseph Shemesh] [609.99s] Secondly, everybody who sit here has have already have already plaque in his coronaries.
[Joseph Shemesh] [618.95s] It's come from the, IVU study on transplanted heart that show us that the teenagers, one of 6, already have signs of atherosclerosis, and they transplanted healthy heart in 50 years, all of them has signs.
[Joseph Shemesh] [636.30s] But everybody his own own rate of acceleration of the atherosclerosis.
[Joseph Shemesh] [644.76s] Some died on the age of 100, and they have nothing as they had on 10 years.
[Joseph Shemesh] [650.84s] And some have on the forties, 50, their plan of atherosclerosis.
[Joseph Shemesh] [655.80s] So the future is to look at these genes and to I think so.
[Joseph Shemesh] [661.76s] And maybe the most important, to find the protecting factors, not only the risk factors.
[Michael McConnel] [670.46s] I wanted to get, Doctor.
[Michael McConnel] [671.90s] Fayad to follow-up on that given you've been imaging atherosclerosis, across the the lifespan.
[Michael McConnel] [678.46s] And and, also, you know, are there opportunities from low dose CT to look at additional information beyond the calcification?
[Michael McConnel] [687.02s] There's sort of pericorn pericornary fat and other things that may give more around the biologic activity and risk for progression.
[Zahi Fayad] [696.97s] Yep.
[Zahi Fayad] [697.05s] Yeah.
[Zahi Fayad] [697.37s] So that's very true.
[Zahi Fayad] [698.65s] The aspect of the data coming from PDU, you know, the development of atherosclerosis.
[Zahi Fayad] [702.81s] Nasiv knows this very well in terms of its development.
[Zahi Fayad] [705.93s] So this is something that occurs early on.
[Zahi Fayad] [709.17s] And there's obviously something that we're not talking you just mentioned the the molecular activity.
[Zahi Fayad] [714.93s] You know, inflammation is one of them, but there are also opportunities for other signatures.
[Zahi Fayad] [720.93s] So right now, I think with the low dose, imaging that we have, it will be hard to get molecular activity, you know, from these images, but they could be other surrogate markers that we still have to validate.
[Zahi Fayad] [736.46s] One of them, as you mentioned, is a very, you know, coronary, very artery fat accumulation.
[Zahi Fayad] [741.99s] That's not a direct measure of inflammation, but it could be an indirect measure.
[Zahi Fayad] [747.02s] I think there is an opportunity to look at that.
[Zahi Fayad] [749.85s] But I also think that, you know, beyond I mean, although I'm an imager, but I'm also looking at other markers beyond imaging.
[Zahi Fayad] [756.65s] There are things in the blood, and especially in the future, we may be able to measure a point of care measurement of blood in a frequent manner, and then, you know, it's getting cheaper to analyze one of these proteins.
[Zahi Fayad] [768.87s] So we could come up with a signature.
[Zahi Fayad] [771.11s] There's a combination of imaging as well as other markers, and then the third one is the aspect of physiology and using, as you know very well, wearables and other type of sensors to put them all in combination.
[Zahi Fayad] [784.79s] I mean, more and more, I'm I'm starting to, you know, rethink, of my origin, which is in electrical engineering.
[Zahi Fayad] [791.63s] That it's very hard to rely on just one marker to try to diagnose a problem when you're looking at a at a at a computer board, and you're trying to figure out is this is this working?
[Zahi Fayad] [801.88s] What what is the issue with this?
[Zahi Fayad] [803.79s] You need a combination of markers, and I think, Deepak, you alluded to in some of your motivation monitoring aspect.
[Zahi Fayad] [811.21s] You mentioned the ear only, looking at voice, which is another one.
[Zahi Fayad] [815.61s] And I know Mark presented a very beautiful concept, which is that combination of things.
[Zahi Fayad] [821.36s] So I I would like to take the discussion beyond the imaging.
[David Maron] [826.24s] There's so many things to discuss.
[David Maron] [829.91s] I don't wanna take it away from imaging for a moment.
[David Maron] [833.15s] And, I'd like, Nathan Wong and, others who would like to chime in to talk about the impact of the patient seeing their disease, and in the case of coronary calcium, seeing calcified plaque, and what the impact can be in in terms of patient adherence, persistence, motivation?
[Nathan Wong] [863.13s] Yeah.
[Nathan Wong] [863.37s] That's a wonderful question, David.
[Nathan Wong] [865.21s] And and I also wanna get back to your original question about, you know, are we there yet, and do we need a randomized trial?
[Nathan Wong] [872.09s] But, yeah, with respect to the question of, you know, is a picture worth a 1000 words.
[Nathan Wong] [877.84s] Right?
[Nathan Wong] [878.31s] So, we, published one of the original studies looking at this with coronary calcium back in 1996.
[Nathan Wong] [888.00s] So, like, 26 28 years ago, I guess it was.
[Nathan Wong] [892.64s] So what we showed, and this was based on a cohort of people that, got coronary calcium scan in the Los Angeles Los Angeles area when they had these Heart Trek America screening programs, you know, that some of you may remember from from from the late eighties early nineties.
[Nathan Wong] [913.80s] But what we showed was that, we surveyed people who who got calcium scans, and those who were scanned, and particularly if their scores were higher, were, shown to be reported.
[Nathan Wong] [929.63s] They were more likely to, to, like, follow a healthy diet, start cholesterol lowering medicine, see their doctor even as well as other preventive behaviors.
[Nathan Wong] [941.62s] And then, you may also recall the Eisner study that, Dan Berman and I were involved with.
[Nathan Wong] [948.26s] And that was actually the first randomized trial of calcium scan and versus no scan.
[Nathan Wong] [954.26s] And that also showed not only improved behaviors, but it showed that people who got scanned actually halted their progression in Framingham risk score, whereas the people who are not scanned actually had an increased score.
[Nathan Wong] [971.10s] But that study, study, being done in the fairly healthy Beverly Hills type population around Cedars Sinai didn't, have enough events to show that event prediction was important.
[Nathan Wong] [984.10s] So, you know, kind of back to your question, and, you know, I think we've all been concerned that the preventive health services task force is really insisting on randomized trials.
[Nathan Wong] [996.46s] You know?
[Nathan Wong] [996.95s] Of course, there's the, the since since which was published a few years ago, which dismissed its primary endpoint, which, actually, they looked at total mortality, and most of us feel that they should have looked at at, you know, like MACE, you know, and and all cardiovascular events.
[Nathan Wong] [1023.35s] And they recently did a, did a secondary analysis looking at what they call patient, you know, patient, preferred outcomes and where they surveyed patients about what outcomes they felt were most important.
[Nathan Wong] [1041.91s] So so the patients felt that, you know, like the usual MACE outcomes, MI, stroke, and cardiovascular death are most important.
[Nathan Wong] [1050.85s] And when you looked at that composite, there actually was a significant benefit.
[Nathan Wong] [1055.09s] But we're still waiting, of course, for the, actually, for the Robinska trial.
[Nathan Wong] [1060.98s] That's gonna be most definitive in showing whether calcium scan improves improves outcomes over the long term.
[David Maron] [1069.94s] So we're gonna go into that.
[David Maron] [1071.38s] Dan, can have us published too early.
[David Maron] [1073.31s] Their their primary endpoint is called for 10 years.
[David Maron] [1075.79s] They they published too early and and blew it.
[David Maron] [1080.27s] Roxanna, when you see patients, do you show them
[Roxana Mehran] [1083.87s] Yes.
[David Maron] [1084.52s] Images?
[Roxana Mehran] [1085.42s] Yes.
[Roxana Mehran] [1085.58s] I pull it up.
[Roxana Mehran] [1086.38s] It's really I learned that from Vivek Reddy because when he, in every I I was I was lucky enough to be in Vivek's, clinic because that we shared clinic space, and I saw that every EP patient is seeing what atrial fibrillation looks like, what is it doing, what what's going on with the pathways.
[Roxana Mehran] [1108.71s] He shows these beautiful cartoons.
[Roxana Mehran] [1110.87s] And so now I do the same, and then I show them and here's what the CAT scan does and here's what yours looks like.
[Roxana Mehran] [1116.93s] And it does make a difference.
[Roxana Mehran] [1118.21s] And I don't know that what the the unknowns and the intangibles are the change in behavior and how that has an impact on ad not just adherence, but actual change in the biology.
[Roxana Mehran] [1129.97s] We don't understand that at all, and it's really exciting to see.
[Michael McConnel] [1134.86s] I wanna follow-up with doctor Reddy.
[Michael McConnel] [1136.62s] We had a little bit of, email conversation in advance, and I know you indicated it in your talk.
[Michael McConnel] [1143.70s] But this idea that Moritz originally showed of, you know, looking at any one characteristic and to doctor Fayad's point, we have multiple sources of data.
[Michael McConnel] [1155.98s] The concept of looking at the underlying sort of vulnerable structure with large atria that you can see on a low dose CT in combination with do they have a vulnerable characteristic of their rhythm and an underlying vulnerable patient, with CHAD VAS scores and things like that.
[Michael McConnel] [1174.68s] So, yeah, how do you see us moving forward on really, how do we optimize that early detection, but who's really gonna benefit from the intervention, which is what we're, you know, at the end of the day, what we most care about.
[Vivek Reddy] [1188.62s] Yeah.
[Vivek Reddy] [1189.41s] I'm gonna be a little bit doted.
[Vivek Reddy] [1190.93s] I apologize for that.
[Vivek Reddy] [1191.98s] But, you know, about a decade ago, we thought that just identifying afib was sufficient and would improve outcomes.
[Vivek Reddy] [1199.23s] And what we rapidly learned was, no.
[Vivek Reddy] [1201.47s] We can identify afib, but what happens is that, you know, in fact, if you just did a study where we took anybody walking on the street and you randomized them to giving an anticoagulant versus not, if you did a big enough study, let's say, a 1000000000 patients, you would see a reduction in stroke probably.
[Vivek Reddy] [1219.17s] The problem is you paid 2 penalties, 2 costs.
[Vivek Reddy] [1221.82s] 1 is the cost of bleeding, which is a substantial one, and we know from the from the coronary studies and other studies that bleeding means death.
[Vivek Reddy] [1230.45s] And the second cost is actually cost itself.
[Vivek Reddy] [1233.01s] I mean, these are expensive therapies, and there's a cost analysis that becomes critical.
[Vivek Reddy] [1237.01s] So in the past, we've really just looked at clinical predictors and CHA2DS2 Vascular, for example.
[Vivek Reddy] [1242.95s] I was just say clinical risk, predictors of, morbidity, plus whether or not there's AFib and maybe how much there AFib that there is.
[Vivek Reddy] [1251.93s] Now it's very clear that we need at least 1 and probably multiple other dimensions, whether that's an imaging dimension, a functional dimension, a, humoral biomarker dimension.
[Vivek Reddy] [1263.77s] And the the complexity here is that we're talking about a we're talking about improving outcomes in where we're talking about potentially treating a lot of patients.
[Vivek Reddy] [1273.80s] So there's both the the cost and the complexity of whatever that third dimension is.
[Vivek Reddy] [1278.99s] So it could be a fantastic test, but if it costs a lot of money to do the test and it's hard to implement in practice, it's not gonna charge out change outcomes on a population level.
[Vivek Reddy] [1289.11s] And then so I think that's where the complexity is.
[Vivek Reddy] [1293.11s] You know, there's I sort of alluded to a little bit.
[Vivek Reddy] [1295.75s] There's, I think, some optimism to think that I'm sorry.
[Vivek Reddy] [1300.79s] There's one last issue, which is then implementing this in clinical practice.
[Vivek Reddy] [1304.63s] Right?
[Vivek Reddy] [1305.42s] Just the CHA2DS2 VASc score, which is not a particularly complex score, is very hard to implement that in clinical practice.
[Vivek Reddy] [1311.35s] So how do you then how do you take something that's somewhat complicated, add additional complexity, and incorporate in a clinical practice?
[Vivek Reddy] [1319.36s] And I think that what we're probably moving toward is something where there's some deep learning algorithm that'll help us, you know, correlate the clinical information, scan through, probably the EHR, and hopefully come to, to saying this is a high risk person that'll benefit from OAC or not.
[Vivek Reddy] [1338.30s] But ultimately, and this is my last point, we have to do prospective randomized trials.
[Vivek Reddy] [1342.63s] If we don't see improvements in outcome, it just it's not gonna affect practice.
[Michael McConnel] [1348.15s] Yeah.
[Michael McConnel] [1348.39s] And then as Bob Harrington mentioned, you know, there has to be some financial incentive to actually implement, you know, what we what we learned.
[Michael McConnel] [1358.33s] Doctor Penney, I wanted to I think there's similar challenges and concepts around heart failure.
[Michael McConnel] [1366.28s] You know, there's data from CT scans.
[Michael McConnel] [1369.88s] They're looking at chamber dimensions can be predictive of heart failure.
[Michael McConnel] [1373.80s] It's now been added or prevent risk score from the You know, used to focus on just ASCVD.
[Michael McConnel] [1381.55s] Now there's a heart failure risk, component to it.
[Michael McConnel] [1386.43s] How do we but I think our mindset is still typically you think about heart failure when somebody has their first episode and then manage it from there.
[Michael McConnel] [1395.79s] But, yeah, the this idea of sort of combining risk factors, what we can learn from chamber sizes on, CT and others, How yeah.
[Michael McConnel] [1408.06s] Your thoughts on moving this earlier and what further clinical trials do we need?
[Sean Pinney] [1412.30s] Yeah.
[Sean Pinney] [1412.54s] It's a great question.
[Sean Pinney] [1413.34s] I mean, I was taught many, many years ago that the left atrium is the set rate for the cardiologist.
[Sean Pinney] [1418.54s] So when you see left atrial enlargement, whether it's by a CT scan or, you know, an echocardiogram or by an ultrasound that happens to be done point of care in the emergency department, that identifies already a a patient who's at risk for further clinical progression.
[Sean Pinney] [1432.56s] And that obligates us to go a little bit deeper.
[Sean Pinney] [1435.20s] And so we've heard it many times today that we have to think about things from a pathophysiologic basis.
[Sean Pinney] [1440.81s] When what causes the left atrium to enlarge?
[Sean Pinney] [1443.05s] It's usually higher left ventricular end diastolic pressures or a mitral valve that is leaking.
[Sean Pinney] [1449.22s] So even in asymptomatic patients, it's telling us that there is already structural remodeling, and the first manifestation of it may be that left atrium.
[Sean Pinney] [1457.30s] The downstream consequences of that, it can go down a couple different pathways, can certainly go down a heart failure pathway.
[Sean Pinney] [1463.20s] I'm at elevated ventricular and atrial filling pressures.
[Sean Pinney] [1467.20s] It does not take much more effort than to begin to develop shortness of breath as pulmonary pressures begin to rise.
[Sean Pinney] [1473.92s] But the other thing that can happen is you can go down electrical pathway, and doctor Reddy mentioned this.
[Sean Pinney] [1478.09s] You get atrial remodeling and that leads to electrical remodeling and atrial fibrillation and then consequently stroke.
[Sean Pinney] [1484.49s] So we do not yet have enough information to act solely on an elevated or in a large left atrium.
[Sean Pinney] [1492.12s] But we do have evidence to say that if you have elevated natriuretic peptides as an example of someone who has elevated filling pressures and ventricular strain, ventricular wall strain, and that's an indication to begin treatment.
[Sean Pinney] [1504.31s] That's an indication to begin treatment with a RAS antagonist, and we have data going all the way back from the solve trials, that showed that solved prevention with the introduction of an ACE inhibitor can forestall, and delay the incident heart failure and can also improve survival in patients who do develop symptomatic heart failure.
[Sean Pinney] [1525.81s] What's really tantalizing is to think about the SGLT 2 inhibitors, class of drugs that we haven't talked about today.
[Sean Pinney] [1532.15s] But these cardiometabolic drugs are having profound effects, almost immediate effects on outcomes.
[Sean Pinney] [1538.95s] We can begin to see improvement in cardiovascular event rates within 2 to 4 weeks of starting an SGLT 2 inhibitor.
[Sean Pinney] [1546.32s] And it makes sense then to think that these benefits extend not only to heart failure, but also to atherosclerotic events.
[Sean Pinney] [1552.56s] So I'm a big proponent of of starting them, but I will strike the note of caution that doctor Reddy shared with us, which is that we do need clinical trials, and we do need clinical trials before we can advocate doing it.
[Sean Pinney] [1564.43s] I think the direction and my bias is that they will be helpful, but we need to prove it.
[Michael McConnel] [1571.87s] Yeah.
[Michael McConnel] [1572.67s] I want to ask doctor Mahdi to follow-up on that.
[Michael McConnel] [1576.38s] I mean, one concept because one of the challenges around prevention is the clinical trials often get funded when there's a new drug or a new intervention that's associated with it, which has always been a challenge for prevention.
[Michael McConnel] [1593.46s] But, you know, is a concept that people with a positive coronary calcium score of or of a certain level, they get randomized to an SGLT 2 inhibitor, a GLP 1, to really, you know, give more precise benefits.
[Michael McConnel] [1613.18s] What are your thoughts on how do we evaluate these new drugs in combination with early disease detection?
[Amir Ahmadi] [1620.71s] Thank you.
[Amir Ahmadi] [1622.97s] Not sure about the SGLT2, but I think I take it one step back.
[Amir Ahmadi] [1627.29s] And I think what we are seeing here in this conference and and in this realm of literature is a little bit of a shift in philosophy.
[Amir Ahmadi] [1636.40s] I think the shift in philosophy that we are all talking about is that we are going away from guesstimation to actually seeing early disease.
[Amir Ahmadi] [1645.29s] Specifically with Tres CVD, specifically with coronary disease.
[Amir Ahmadi] [1649.89s] The reason that we practice what we practice is very historical.
[Amir Ahmadi] [1653.81s] And I think what we are really seeing now is that, to me, instead of actually thinking and and completely focusing on blood markers, which are very important.
[Amir Ahmadi] [1664.03s] I'm not saying we shouldn't do that.
[Amir Ahmadi] [1665.87s] Coronary diseases are coronaries.
[Amir Ahmadi] [1668.11s] The the lipid particles that are actually in the vessels of the heart are the ones that cause problem, not the ones that are in the blood.
[Amir Ahmadi] [1677.59s] If there is a relationship that is 1 to 1 from the blood to the heart vessel, great.
[Amir Ahmadi] [1681.83s] But but the relationship is not 1 to 1.
[Amir Ahmadi] [1684.15s] It's much more complex.
[Amir Ahmadi] [1685.83s] So we see this in more of a sub analysis of clinical trials.
[Amir Ahmadi] [1689.99s] For example, you look at the Scott Heart trial, and you look at the patients that have non cardiac symptoms.
[Amir Ahmadi] [1698.58s] In 5 years, they have actually a my benefit.
[Amir Ahmadi] [1701.21s] Just by detection of the very beginning of their classification and starting on statin treatment, They calculate the number for the NNT of the statin treatment in that MI prevention, and it becomes 3.
[Amir Ahmadi] [1714.44s] And people are like, what are you talking about?
[Amir Ahmadi] [1716.52s] Statin cannot have NNT of 3.
[Amir Ahmadi] [1719.00s] And the answer to that is that it's not a statin of NNT.
[Amir Ahmadi] [1723.05s] Is it sorry.
[Amir Ahmadi] [1724.34s] It's not a n and t of the statin.
[Amir Ahmadi] [1726.26s] This is a number needed to treat out of different philosophy.
[Amir Ahmadi] [1729.54s] You're guesstimating in one group and and just putting it based on the ACVD risk score, which is important.
[Amir Ahmadi] [1734.51s] And in the treated.
[Amir Ahmadi] [1739.95s] If you don't see the disease, you're not that committed.
[Amir Ahmadi] [1742.19s] If the person comes with a muscle pain, you are like, okay.
[Amir Ahmadi] [1745.23s] Fine.
[Amir Ahmadi] [1745.71s] Try your other method.
[Amir Ahmadi] [1747.07s] But if you if there is a disease, you're committed to it.
[Amir Ahmadi] [1749.87s] So going back to your question about all of these drugs, I think what is very exciting is a new philosophy.
[Amir Ahmadi] [1756.24s] And I think there are companies and there is industry that that like this philosophy.
[Amir Ahmadi] [1761.77s] And I think what really comes to it as a as a added bonus is this invention of AI.
[Amir Ahmadi] [1767.86s] And I think what we are seeing in image and in CT is one thing that what my eyes and my brain can comprehend.
[Amir Ahmadi] [1774.26s] But in a deep learning model, for example, how to how to relate the calcification and the aortic valve that Rebecca Sharma was talking about with the echocardiography, I'm sure in 10 years, AI would look at the CT and can predict the v max.
[Amir Ahmadi] [1788.72s] And and and I think the industry that is sponsoring that would be very much supportive of sponsoring the trial and the, practical integration.
[David Maron] [1797.68s] Has
[Morteza Naghavi] [1801.49s] his We came here for one big question, and that's the question that doctor Marin asked doctor Harrington, and that's the evidence.
[Morteza Naghavi] [1811.73s] Because if you don't have the evidence right And now the on the piggyback of that is the slide that I asked, if you could bring back that slide.
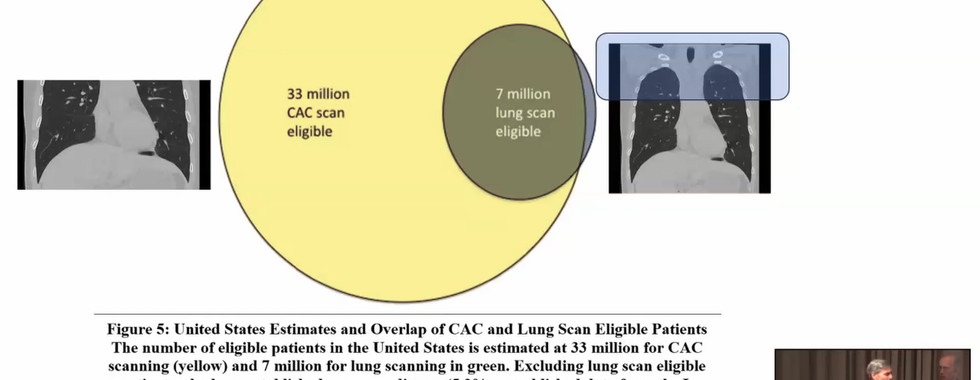
[Morteza Naghavi] [1821.30s] We have a 30 some, 35, 37,000,000, population.
[Morteza Naghavi] [1825.86s] Could you bring, please bring that
[Amir Ahmadi] [1827.78s] as well?
[Morteza Naghavi] [1828.50s] Okay.
[Morteza Naghavi] [1828.74s] Great.
[Morteza Naghavi] [1829.14s] So this the left side, this is a little outdated, but look at it.
[Morteza Naghavi] [1834.86s] It's close to 50 40,000,000 that qualify as part of intermediate risk that would fall under, 2019, 18 guidelines to get coronary calcium scan.
[Morteza Naghavi] [1847.59s] On the right side is the lung cancer population that increased a little bit close to now 10 to 15,000,000.
[Morteza Naghavi] [1856.31s] What we're here, you know, again, trailblazer, we're trying to open a new pathway is that we apply a low dose to the entire population.
[Morteza Naghavi] [1867.33s] We don't have evidence to subject the upper third of the lung to radiation.
[Morteza Naghavi] [1874.28s] So that's one problem.
[Morteza Naghavi] [1875.80s] The second problem is what comes downstream, what happens to those people that are found to have nodules or at a pathology intervention that comes out.
[Morteza Naghavi] [1885.32s] So if you could please help us from this collection of gray matters, we come to some level of direction of is it what so I asked David and Claudia before our meetings.
[Morteza Naghavi] [1899.41s] David said, you know, that 1 third, that actual radiation is equal to 1 at chest x-ray.
[Morteza Naghavi] [1906.16s] Let's just prove that and demonstrate model and so on.
[Morteza Naghavi] [1910.56s] We already have Fleischner algorithms of what to do with why don't we why do we have to launch a new trial for this?
[Morteza Naghavi] [1920.05s] So if you could please, elaborate.
[David Maron] [1922.86s] So I'm I'm going to make an assumption that this is a room of believers, and we need evidence for payers to pay.
[David Maron] [1934.48s] Who's gonna pay for all those scans?
[Morteza Naghavi] [1940.00s] Whoever is paying now for the downstream cost.
[David Maron] [1942.77s] Yeah.
[David Maron] [1943.01s] May maybe we can get one of the presidential candidates to promise to do it.
[David Maron] [1947.96s] Like
[Morteza Naghavi] [1948.29s] We have a we have a Medicare hearing coming up.
[Morteza Naghavi] [1951.57s] This whatever you guys come up with you know, we had 4 hearings.
[Morteza Naghavi] [1954.92s] This is our 5th.
[Morteza Naghavi] [1956.29s] This one is bigger because we're talking about something really large.
[David Maron] [1961.17s] Yeah.
[Morteza Naghavi] [1961.57s] So any thoughts?
[David Maron] [1962.61s] It's well, it, you know, it it's the question I was gonna ask, doctor Amadi, is you showed with the take home point I got from your presentation was that most of the events are occurring in low risk people.
[David Maron] [1977.09s] The radiologists and pulmonologists in the room, they're seeing the high risk people.
[David Maron] [1983.02s] So, yeah, we could start with incidental, but we're missing and sorry using the term incidental.
[David Maron] [1989.62s] I don't know what else to call.
[David Maron] [1992.14s] The buy the buys by bystander findings.
[David Maron] [1997.92s] Where do we go to to find all those low risk people?
[David Maron] [2001.52s] The they're out in the population.
[David Maron] [2004.01s] We need population screening.
[Zahi Fayad] [2007.20s] But, I mean, let me maybe interject here a little bit.
[Zahi Fayad] [2010.16s] I mean, when we say I mean, I was looking at your paradigm and we've been discussing this for a very long time, you know, with Fuster and more and etcetera.
[Zahi Fayad] [2018.79s] You you will find the plaque, but it does not mean that this is actually gonna cause it.
[Zahi Fayad] [2023.58s] I mean, it's it's really we we never found that one to one correlation.
[Zahi Fayad] [2028.38s] It's a burden.
[Zahi Fayad] [2029.82s] It's the whole aspect of it.
[Zahi Fayad] [2031.10s] So maybe you can elaborate a little bit.
[Amir Ahmadi] [2033.73s] I would say it this way.
[Amir Ahmadi] [2034.93s] If you don't have a plaque, you're not at an immediate risk of a mine.
[Amir Ahmadi] [2038.97s] Not actually type 1 MI.
[Amir Ahmadi] [2041.05s] If you do have a plaque, it's kind of like a soccer game that is started and the other team is playing.
[Amir Ahmadi] [2046.73s] If you're not playing against them, you may get scored the ball.
[Amir Ahmadi] [2049.53s] But what what is important is, is I had a slide that I showed detection of plaque, starting of a treatment, progression of a plaque, treatment intensification.
[Amir Ahmadi] [2061.88s] And what we see right now, for example, there is this, new paper came up relatively new in Lancet called orphan trial that, for those of you who are not familiar with this, is is a score of inflammation around the vessel.
[Amir Ahmadi] [2075.78s] It's called the FAI score.
[Amir Ahmadi] [2077.38s] And what they what they showed is a tremendous detection rate.
[Amir Ahmadi] [2081.22s] When you have this inflammation in your vessels that is not one to one related to a systemic inflammation with an event rate if you had non obstructive plaque 2 years prior to that.
[Amir Ahmadi] [2092.64s] So point is, yes, the plaque itself doesn't mean events, but but there are a bunch of other things, as you mentioned, biomarkers and other things and inflammation that can increase that probability and and get us to intensify.
[Zahi Fayad] [2104.33s] May maybe 2 quick comment.
[Zahi Fayad] [2105.77s] I mean, it's a question of really trying to figure out probabilities.
[Amir Ahmadi] [2109.95s] Mean, you know,
[Zahi Fayad] [2110.28s] that's very important is to be able to to do that.
[Zahi Fayad] [2113.80s] The second aspect, you know, related to what you said about phy, which is the inflammation very coronary, that's the same idea also with high sensitivity CRP.
[Zahi Fayad] [2123.57s] It is it is an it is not a marker of exact inflammation.
[Zahi Fayad] [2127.41s] It could be related to this.
[Zahi Fayad] [2128.93s] It may be an integrator of this, and that's what we really have to try to get a little bit more detail.
[Amir Ahmadi] [2134.21s] Right.
[Amir Ahmadi] [2134.45s] Yeah.
[Nathan Wong] [2134.85s] And I think another, you know, thing, paradigm that has to change is we need to, you know, think about staging of atherosclerosis.
[Nathan Wong] [2144.24s] You know, like how we stage them heart failure.
[Nathan Wong] [2147.04s] And, you know, the the PREVENT risk score has made some progress in at least stage in cardiometabolic disease.
[Nathan Wong] [2156.61s] So that's a step in the right direction.
[Nathan Wong] [2158.77s] But and I don't know, David, if you wanna say a little bit about, you know, the stage in stage in paper that is in development.
[David Maron] [2171.61s] It's coming, in the in the next few weeks.
[Speaker 4] [2176.48s] I I would Okay.
[Speaker 4] [2177.61s] Agents.
[Michael McConnel] [2178.32s] Yeah.
[Speaker 4] [2179.36s] It's coming out in a in a publication.
[Speaker 4] [2181.61s] Yeah.
[Speaker 4] [2181.99s] But
[Michael McConnel] [2182.15s] I would say to to Mort's question around when you're talking to agencies and how to get this used more, you know, the guidelines use coronary calcium for, you know, not just a black, you know, black and white broad screening.
[Michael McConnel] [2197.80s] It's much more to give you an athero burden to very directly guide therapy and the patient sitting in front of you, and a chunk will have a score of 0.
[Michael McConnel] [2209.57s] And then the guidelines align coronary calcium score burden with degree of LDL lowering.
[Michael McConnel] [2217.94s] So I think presenting it as not just a sort of broad yes or no, but it helps refine, optimize, personalized, and it and will sell.
[Michael McConnel] [2228.53s] Some people don't need to go on therapy and others who need
[Morteza Naghavi] [2231.57s] to be more on.
[Morteza Naghavi] [2232.93s] They don't need.
[Morteza Naghavi] [2233.82s] So doctor Fuster and I went straight to Maryland to CMS and sat down in front of the director of, coverage.
[Morteza Naghavi] [2243.85s] And, you know, with his way of talking, he was saying, you have to also look at this CAC 0, the CAC 0 population unburden, unnecessary treatment that you have.
[Morteza Naghavi] [2255.53s] Currently, you're paying for it.
[Morteza Naghavi] [2257.45s] You're already paying for it.
[Morteza Naghavi] [2259.05s] So if you can undo a significant investment that you're doing here and direct it to those who have CAC over 100 and high risk, you don't we're not asking you to cuff out more money to the system.
[Morteza Naghavi] [2274.50s] We're asking you to shift investment in primary prevention guided by imaging.
[Morteza Naghavi] [2281.14s] So that's where we left it a lower cost if we if we do it properly.
[Morteza Naghavi] [2287.78s] Now in the same image, we now are showing with AI a bunch of other things that can predict heart failure because we know calcium score sucks at predicting heart failure or atrial fibrillation and possibly some of these markers of fat related linked to inflammation.
[Morteza Naghavi] [2306.25s] So, you know, this was their dream.
[Morteza Naghavi] [2309.13s] Claudia and David started this.
[Morteza Naghavi] [2311.21s] They published this.
[Morteza Naghavi] [2312.01s] I wasn't even collaborating with them when they published this.
[Morteza Naghavi] [2315.76s] But now this stream is really close to reality with AI without adding cost.
[Morteza Naghavi] [2322.64s] So but as experts, we have to define the downstream.
[Morteza Naghavi] [2327.34s] Because if you put this on, you know, as you know, in Pernuva or somebody in body MRI, people go get the MRI, and a majority of them have something.
[Morteza Naghavi] [2336.14s] And if there is no well thought out plan on what to do with the downstream findings causing anxiety, causing unnecessary interventions, and so on, we wouldn't do our job.
[Morteza Naghavi] [2348.95s] People want to improve health care.
[Morteza Naghavi] [2350.64s] We're just making it probably worse.
[Morteza Naghavi] [2352.68s] So if you could please elaborate in that with our panel.
[Morteza Naghavi] [2359.48s] So 2 two sides.
[Morteza Naghavi] [2361.32s] The extra burden of radiation and then the downstream intervention that it causes or you know, I don't like his incidental finding reference, but opportunity finding whatever.
[Morteza Naghavi] [2373.84s] How do we see that coming together?
[David Maron] [2378.40s] Well, it it could take a while to to truly respond.
[David Maron] [2384.90s] I would say that if we did dual screening so if we're screening for lung cancer or other lung diseases, at the same time that we're screening for cardiovascular disease, that we, number 1, make it more attractive to those people who should be screened, who are not being screened so that they can get, for example, a coronary calcium score, which is typically only ordered for people at higher socioeconomic or higher education levels.
[David Maron] [2425.56s] So it would open it up to more marginalized populations who are not taking advantage of lung cancer screening, which is generally paid for.
[David Maron] [2437.41s] So that is one way to really open things up.
[David Maron] [2443.97s] But I don't know anything.
[David Maron] [2446.61s] Do do you have some intelligent response to, what doctor Nagavy said?
[Speaker 4] [2450.69s] Yeah.
[David Maron] [2450.86s] Does somebody on the panel would someone on the panel yes.
[David Maron] [2453.26s] Doctor Shemesh.
[Joseph Shemesh] [2454.69s] I think that, all the change of imaging, early imaging of atherosclerosis, it's it's not by itself.
[Joseph Shemesh] [2462.69s] It goes by the clinical picture, who is the patient.
[Joseph Shemesh] [2466.87s] And if you talk about downstream, you are not doing it only just because it has a a calcium score of of 1,000.
[Joseph Shemesh] [2474.31s] You are looking at the at the clinical presentation.
[Joseph Shemesh] [2477.27s] Some of them are doing very well, and the others, if there are some chest pain presentation or what, but what I'm trying to say that if you put and if you use, the the calcium score as a as a as a one more information, very important information to your clinical patient.
[Joseph Shemesh] [2501.39s] Who is the patient?
[Joseph Shemesh] [2503.31s] What are the others, diseases that he have?
[Joseph Shemesh] [2506.59s] What other risk factor that he has?
[Joseph Shemesh] [2508.82s] There are maybe 13 of them.
[Joseph Shemesh] [2510.99s] And then if you took altogether, then you reduce the number to treat.
[Joseph Shemesh] [2516.43s] You treat only those with the high risk and the mesa risk and the PCA risk that algorithms that use the clinical picture with the calcium score gives you the answer.
[Joseph Shemesh] [2532.14s] If and and you have a numeric answer.
[Joseph Shemesh] [2535.09s] 5 less than 5%, you don't have to treat.
[Joseph Shemesh] [2538.38s] And, above 7 and and the and a half percent should you have to treat.
[Joseph Shemesh] [2543.64s] And above 20%, you have to put all your effort and to treat there.
[Joseph Shemesh] [2548.76s] So for the moment, all the things of soft plaque and all the this inflammation, this is for the future.
[Joseph Shemesh] [2557.24s] But when we are going home, the the take home messages is the culture score because it is well, well, well documented, and you can use it.
[Joseph Shemesh] [2567.93s] And the way to use it is to adapt it to the clinical presentation of your patient.
[Joseph Shemesh] [2574.73s] It's not something, oh, I found calcium score what to do.
[Joseph Shemesh] [2578.33s] The the question is the clinical presentation of the patient.
[Nathan Wong] [2582.49s] Yeah.
[Nathan Wong] [2582.81s] And if I could also comment briefly that, you know, with respect to the, actually downstream test in question, you know, at least with the Eisner study and I believe also with Scott Hart.
[Nathan Wong] [2594.77s] Right?
[Nathan Wong] [2595.09s] There there was no increase in downstream testing.
[Nathan Wong] [2599.49s] So so so so I think that's a very important point.
[Nathan Wong] [2602.97s] And then lastly, one thing that we haven't touched on, and maybe, Roxanna or someone might wanna comment on this too, is there's a huge opportunity also with, actually mammograms, which are, you know, because, you know, you're able to detect, you know, actually breast arterial calcification that has been shown to be associated with increased cardiovascular risk, and perhaps those women can then be further evaluated for their cardiac risk.
[Roxana Mehran] [2634.09s] You know, I thank you for bringing that up, and I think it's the power of AI again kind of, in in play with looking at and especially understanding how we're underdiagnosing, undertreating, and underappreciating cardiovascular disease in women.
[Roxana Mehran] [2650.39s] And, the very popular, and well adhered to screening for breast cancer in women allows you the opportunity to evaluate for, breast calcification and its relationship to coronary calcification and cardiovascular disease, and that's work that's being done.
[Roxana Mehran] [2672.57s] But we still need millions and millions more data data points to really, really prove that.
[Roxana Mehran] [2677.84s] But I believe this is a tremendous opportunity for this interdisciplinary imaging AI work and deep learning for us to to not speak in silos, and I think this is what this, congress is all about is exchanging information with each other and finding opportunities when there are when a patient is it's what I what I often think about is if you're bringing the patient in, they're losing their entire day, you're doing a screening, imaging, that their, companies are paying for, then use every opportunity to at least get as much information out of this as possible.
[Roxana Mehran] [2718.12s] So I think it's an it's an opportunity.
[Michael McConnel] [2720.52s] Yeah.
[Michael McConnel] [2720.68s] I have one key point in in the book where I say if you've had a chest CT, a mammogram, or a retinal image and a disclosure, I work for help an AI company doing analyzing retinal images, but make sure they're reviewed for seeing coronary disease, breast artery calcification, or, you know, hypertensive diabetic retinopathy as increased risk.
[Michael McConnel] [2744.02s] So, David, yes?
[David Yankelevitz] [2745.74s] Yeah.
[David Yankelevitz] [2745.90s] I have a comment or 2.
[David Yankelevitz] [2748.54s] 1st, in line with what Roxanna in in terms of sort of siloing, this we've done 46 conferences.
[David Yankelevitz] [2756.94s] We have never had a cardiology panel or discussion like this.
[David Yankelevitz] [2760.73s] This was absolutely spectacular.
[David Yankelevitz] [2763.21s] And and I think this is really as I said, this is gonna be the inflection point where we're really gonna see the integration of cardiology and into the lung screening and vice versa and and a much more holistic approach.
[David Yankelevitz] [2776.11s] So I am delighted, with this panel discussion.
[David Yankelevitz] [2779.87s] The second piece of this, because I'm I'm getting texts from China right now from my former fellow who is watching this very intense, who did work with us on the aortic stenosis.
[David Yankelevitz] [2791.93s] And, you know, it's this kind of thing.
[David Yankelevitz] [2794.09s] We find a fair amount of a we developed an ordinal score for aortic stenosis.
[David Yankelevitz] [2799.14s] And she just reminded me that severe aortic stenosis with our ordinal score was 0.2%, but moderate aortic stenosis recorded almost 2%.
[David Yankelevitz] [2811.61s] It's an enormous number.
[David Yankelevitz] [2813.78s] How many people do we think now?
[David Yankelevitz] [2815.22s] I don't know yet.
[David Yankelevitz] [2816.26s] I have to check because it's really important for us to do this, are acting on any of this information.
[David Yankelevitz] [2821.30s] We know, for example, we did go back and look at, for example, we looked at we report COP we report emphysema on all our scans.
[David Yankelevitz] [2828.52s] We went back and ultimately check how many people knew they had emphysema.
[David Yankelevitz] [2832.76s] It doesn't get disseminated.
[David Yankelevitz] [2834.68s] Different people, you know, and I suspect when we report all these cardiac findings, nobody's looking at them.
[David Yankelevitz] [2840.09s] I report severe aorta stenosis.
[David Yankelevitz] [2842.41s] I doubt that the majority of them are are working it up.
[David Yankelevitz] [2845.14s] So, again, it's almost another level of siloing that we have to figure out how to get this information out and make
[Roxana Mehran] [2851.06s] sure it's changing.
[Roxana Mehran] [2851.70s] Heart is gonna change this because now these people are seeing everything and asking about every question.
[Roxana Mehran] [2858.66s] So I think my chart is a very big step forward.
[Michael McConnel] [2863.14s] So I think we it looks like we have about 7 minutes left.
[Michael McConnel] [2867.14s] Sounds like why don't we hear from Claudia?
[Michael McConnel] [2870.30s] And I know we've been, delinquent about having the audience ask a few questions, but, Claudia, go ahead.
[Michael McConnel4] [2876.30s] So I just wanna say or bring out what you said, that talking to the patient is really very important, and that communication and we we need to jointly do that more so that we communicate.
[Michael McConnel4] [2892.03s] We
[Roxana Mehran] [2892.67s] But we're not talking to our patients anymore.
[Roxana Mehran] [2895.15s] We're typing on computers.
[Roxana Mehran] [2897.14s] We're not using our stethoscope.
[Roxana Mehran] [2898.91s] We're not sitting at eye level.
[Roxana Mehran] [2900.66s] We're not asking the patient, what's going on in your life?
[Roxana Mehran] [2904.18s] Tell me about your stress.
[Roxana Mehran] [2905.78s] That's why I was late because I literally literally this is what I do.
[Roxana Mehran] [2909.78s] I spend a lot of time with patients because I believe that that is the opportunity for you to actually intervene and let that patient feel like someone cares about me.
[Roxana Mehran] [2922.91s] I need to figure out how to care for myself.
[Michael McConnel4] [2925.32s] So let's say it for women.
[Michael McConnel4] [2927.16s] I call patients because I would call the referring physician.
[Michael McConnel4] [2930.99s] I'd say, do you talk to do you wanna talk to the patient, or do you want me to talk to and they, in New York City, they said, oh, you talk to the patient, and I talked to them about and showed them their CT scan.
[Michael McConnel4] [2943.06s] And they would call me and say, thank you so much.
[Michael McConnel4] [2946.26s] When I walked across the street and I started to light my cigarette, I thought of that CT scan that you showed me, and it was that there's tremendous information.
[Michael McConnel4] [2956.91s] We talk about AI and so on, but it's that communication facilitating the communication with the patient, and here's something that you need to think about.
[Michael McConnel4] [2965.76s] And that's what I think Morta's trying
[Speaker 4] [2967.76s] to do.
[Speaker 4] [2968.40s] But our app,
[Morteza Naghavi] [2969.28s] our plan is to make it
[Speaker 4] [2972.72s] that the patient gets it faster than the radiology.
[Speaker 4] [2975.76s] That much.
[Speaker 4] [2976.48s] That fast.
[Speaker 4] [2977.76s] AR does it.
[Speaker 4] [2978.78s] It says pending radiologist approval, but
[Morteza Naghavi] [2983.65s] it's already in their app before they get home.
[Morteza Naghavi] [2987.73s] That's the goal that that's what we hope to get our page to buy into it.
[Morteza Naghavi] [2992.54s] But we have this big question in front of us whether we have the evidence to improve to to implement it.
[Morteza Naghavi] [2999.50s] Claudio's suggestions in our team is that we go to our page and say, we're gonna run this with consent.
[Morteza Naghavi] [3006.13s] So we just disclose that this is a research.
[Morteza Naghavi] [3008.93s] We're going to collect data, maybe, you know, 500,000 patients or a 1000000 patients, but we implemented the research, project.
[Morteza Naghavi] [3018.36s] Please go ahead around the room.
[Michael McConnel] [3020.24s] Yeah.
[Michael McConnel] [3020.48s] If you maybe pass behind you.
[Michael McConnel] [3023.20s] Yeah.
[Michael McConnel] [3024.48s] Yes.
[Michael McConnel] [3025.60s] I And others raise your hand as you're yeah.
[David Yankelevitz] [3028.64s] Just quick quick quick quick point.
[Michael McConnel5] [3030.56s] I'm a radiologist, and I read a lot of these screening CTs.
[Michael McConnel5] [3033.68s] I think something that we're not explicitly saying but we should and something that's already happening on all of these screening CTs is a very understandable recommendation at the end of every CAT scan, which says, like, for the calcium score, we say our or your ordinal calcium score is 8.
[Michael McConnel5] [3048.96s] That means that you're at risk for coronary artery disease and you should see a cardiologist to address your risk factors.
[Michael McConnel5] [3053.76s] Right?
[Michael McConnel5] [3054.00s] It's a standard macro that comes on all of our CTs.
[Michael McConnel5] [3056.88s] Similarly, we could say I say the same thing for aortic valve calcification.
[Michael McConnel5] [3060.48s] Especially in a younger patient, I might say this may represent bicuspid aortic valve.
[Michael McConnel5] [3064.18s] I clearly say, go see your cardiologist and get further imaging.
[Michael McConnel5] [3067.55s] So I think very often, radiologists say things that aren't understood by the patient or the referring doctor, for instance, which is that there's moderate aortic valve calcifications, period.
[Amir Ahmadi] [3077.10s] Well, what does
[Michael McConnel5] [3077.50s] that mean?
[Michael McConnel5] [3078.46s] Right?
[Michael McConnel5] [3078.78s] That's, I think, a a big step forward.
[Michael McConnel] [3083.02s] Yes.
[Michael McConnel6] [3085.02s] Fred Gwyneth, as a retired thoracic surgeon, this was a spectacular review of of adult cardiac disease.
[Michael McConnel6] [3091.20s] And congratulations to everybody.
[Michael McConnel6] [3093.45s] One question I didn't hear is the proof that calcium and plaque are equal to each other.
[Michael McConnel6] [3101.53s] And I would think that there would be a time when plaques begin to become calcified.
[Michael McConnel6] [3107.34s] But what evidence is there to link calcium to plaques?
[Michael McConnel] [3113.10s] So we do actually have a little bit more on this at a session tomorrow morning,
[Speaker 4] [3119.93s] but
[Michael McConnel] [3120.41s] and others can chime in.
[Speaker 4] [3121.93s] I have
[Michael McConnel] [3122.09s] also Yes.
[Michael McConnel] [3123.45s] Go.
[Joseph Shemesh] [3124.81s] Classification of the plaque is some kind of healing.
[Joseph Shemesh] [3128.72s] And it, Peter Libby shows very nicely that high proportion high, dosage of, statin of 80 milligram when he compared it to 40 milligram in IVUS.
[Joseph Shemesh] [3142.17s] He show that the this has increased the calcification and reduced the acute event.
[Joseph Shemesh] [3149.89s] So what we believe now for your question, what is the calcium is doing there?
[Joseph Shemesh] [3154.61s] It's some kind of healing like every chronic inflammatory disease that we have, like, tuberculoma, like, ethnococcus, like, in the shoulder, you see always calcification in a area of chronic long standing inflammation.
[Joseph Shemesh] [3174.84s] And the I we do we do believe, and a lot of researcher thinks so, that calcification is stabilization and some kind of healing of the plaque.
[Nathan Wong] [3186.55s] Yeah.
[Nathan Wong] [3186.78s] But I think we also know that it is it is a powerful marker of the overall burden of atherosclerosis from numerous, numerous angiographic comparison studies done over the last 30 years.
[Nathan Wong] [3203.11s] Right?
[Nathan Wong] [3203.43s] And if you have a high calcium score, there's a great probability that somewhere, not not at the site of coronary calcium necessarily, but somewhere, you are likely to have an obstructive, you know, an obstructive plaque.
[David Maron] [3219.98s] And just for clarification, it it be oh, definitely patient handout.
[David Maron] [3228.94s] Yes.
[David Maron] [3230.22s] I I I would bet that doctor Wong has it.
[David Maron] [3232.46s] I I just wanna make one clarifying remark.
[David Maron] [3235.16s] The the plaque doesn't begin as calcified.
[David Maron] [3238.20s] It begins as non calcified plaque.
[David Maron] [3240.84s] And over time, it becomes calcified, and it's really nice that it gets calcified so that we can see it noninvasively and get an indication.
[David Maron] [3248.04s] But there are people walking out there who have atherosclerosis that don't have any calcification.
[David Maron] [3254.30s] They have noncalcified plaque.
[David Maron] [3255.82s] With aggressive treatment, the noncalcified plaque volume diminishes and the calcified plaque increases, and increases in density.
[David Maron] [3266.39s] Doctor, really quick, we have 59 seconds.
[Amir Ahmadi] [3270.64s] To to go back to Doctor.
[Amir Ahmadi] [3272.32s] Nagami's point as as to what next step is needed.
[Amir Ahmadi] [3275.52s] I think one of the missing point that we have in this is not just to screen, but what to do with the information of screen in terms of treatment.
[Amir Ahmadi] [3283.60s] And I think within the community of cardiology, we don't have a unifying answer to that.
[Amir Ahmadi] [3289.44s] One of the things that I tried to mention is that diseases start with plaque, ends with plaque rupture in between its progression.
[Amir Ahmadi] [3297.26s] The reason that we have a secondary prevention guidelines is that we know that around the early of 60 or 70, we can stop progression.
[Amir Ahmadi] [3305.82s] But I'm not entirely sure if all the cardiologists, if c calcium score of 1, they bring the LDL less than 70.
[Amir Ahmadi] [3312.78s] If we do that, we actually see event reduction.
[Amir Ahmadi] [3315.42s] If we see event reduction, we have NNTs.
[Amir Ahmadi] [3317.74s] We have NNTs.
[Amir Ahmadi] [3318.86s] We have cost calculations.
[Amir Ahmadi] [3320.53s] We've had that in a 2,000 patient population in a practice that I was involved.
[Amir Ahmadi] [3325.41s] And the cost of MI prevention would be under $20,000 in a 7 year follow-up.
[Amir Ahmadi] [3332.30s] And I think that's in a larger scale what what we really need.
[Amir Ahmadi] [3335.58s] But but currently, there is a little bit of a confusion as to what to do with these numbers.
[Speaker 4] [3340.46s] Yeah.
[Speaker 4] [3341.18s] That's what we're we are proposing to r by h that find a disease that occurs for us as positive, negative now Like, you know It's fine.
[Speaker 4] [3350.74s] 1205.
[Speaker 4] [3352.26s] And then new intervention and put a very clear boundary.
[Speaker 4] [3356.11s] No additional testing.
[Speaker 4] [3357.39s] Exactly.
[Morteza Naghavi] [3358.03s] So don't spend another $1,000 on a nuclear
[Speaker 4] [3362.18s] or a lifeblood.
[Speaker 4] [3363.56s] Get this patient on a cheap, established treatment, you know, $20, you know, $30 a year.
[Speaker 4] [3370.20s] We have that and be able to improve often.
[Speaker 4] [3373.80s] So I think this is the the the hope we have for this session.
[Speaker 4] [3377.91s] To bring it up, we knew that we could not finish it.
[Speaker 4] [3380.39s] Claudia said, the only hope hope life.
[Speaker 4] [3382.39s] Your expectation are you will have a hope.
[Speaker 4] [3384.88s] We are going as I showed you this, reshaped working group.
[Speaker 4] [3389.96s] We're going to communicate with you, all of you in this panel, for a riot, just like we did with our first shade passport report.
[Speaker 4] [3398.04s] This would be the first of long and hard.
[Speaker 4] [3400.76s] So it's really exciting.
[Speaker 4] [3402.28s] 20 years ago, I think that the shade that we're going to
[Joseph Shemesh] [3405.64s] do it
[Speaker 4] [3407.05s] And nothing changed since.
[Speaker 4] [3408.93s] Yeah.
[Speaker 4] [3409.17s] A lot of times changed.
[Speaker 4] [3410.69s] Yes.
[Roxana Mehran] [3411.17s] It's been a funny year.
[Roxana Mehran] [3412.61s] Really reshaped many, many things.
[Roxana Mehran] [3414.45s] I'm I'm gonna say a lot has changed.
[Speaker 4] [3417.11s] Yeah.
[Speaker 4] [3417.75s] So exactly.
[Speaker 4] [3419.27s] Messy.
[Morteza Naghavi] [3421.83s] Firm reshape based on this.
[Morteza Naghavi] [3424.07s] And I, honor that.
[Speaker 4] [3425.99s] And we're going to communicate with you for a right number.
[Amir Ahmadi] [3429.51s] Then it's safe.
[Zahi Fayad] [3430.68s] Yep.
[Zahi Fayad] [3430.84s] In
[Roxana Mehran] [3431.72s] shade.
[Roxana Mehran] [3431.89s] Then in shade.
[David Yankelevitz] [3432.45s] Yeah.
[David Yankelevitz] [3432.93s] So so this
[David Yankelevitz] [3435.09s] this was the introduction of cardiology to the lung community.
[David Yankelevitz] [3440.36s] The next session will be the lung community introducing our issues to the cardiac community.
[David Yankelevitz] [3447.10s] We have a pretty tough tall order to to meet the quality that we saw today.
[David Yankelevitz] [3451.02s] So I just wanna thank the panelists and the moderators for what I think was just a spectacular set..
The presentations were hosted by I-ELCAP – The International Early Lung Cancer Action Program.
















Comments